A UK evaluation of rare incidents in which primary care provided by telephone or video has ended with the death or serious harm to a patient provides insights into what can be done to make sure use of virtual care remains safe.
The study published in BMJ Quality and Safety evaluated 95 serious safety incidents involving what the researchers call remote interactions between 2015 and 2023. The study also evaluated the use of virtual care in a diverse range of 12 general practices throughout the United Kingdom from mid-2021 to the end of 2023.
Many reports of the study published in general UK media have focused on the downside of virtual care. For example, the Daily Mail had a headline saying, “Patients are ‘dying from remote GP consultations as major study warns virtual and phone appointments can miss serious illnesses.” However, the study authors repeatedly note throughout the article the rarity of serious adverse events associated with virtual care.
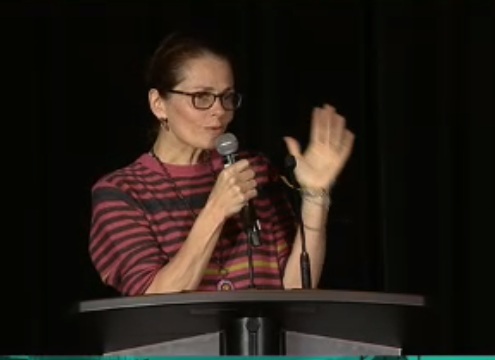
Writing on the social media platform Bluesky, Dr. Trish Greenhalgh, one of the study authors and professor of primary care sciences at Oxford University states: “this paper is MAINLY (emphasis hers) about how remote care in GP land is remarkably SAFE. We followed 12 GP practices for 2y, looking for (among other things) evidence of patient harm from remote consultations. We found NONE.”
In an associated post, she added: “a BIG finding from this study was how safety incidents are almost always AVOIDED through the conscientious actions of front-line staff (from receptionists to senior docs).”
In their analysis of the series of safety issues associated with remote care, authors of the study identify a wide range of contributing factors especially at the system level.
“Introduction of remote triage and expansion of remote consultations in UK primary care occurred at a time of unprecedented system stress (an understaffed and chronically under-resourced primary care sector, attempting to cope with a pandemic),” the study notes.
System issues associated with adverse events and identified in the analysis include:
- Technically complex access routes which patients found difficult or impossible to navigate requiring non-clinical staff to make clinical or clinically related judgements.
- High demand, staff shortages and high turnover of clinical and support staff making remote encounters inherently risky.
- Single episodes of care for one problem often involving multiple encounters or tasks distributed among clinical and non-clinical staff
- Not sufficiently adapting organizational routines to virtual care
- Training, supervising, and inducting staff being made more difficult when many were working remotely.
- Communication is singled out as an important factor associated with adverse events and virtual care.
“Many safety incidents were characterised by insufficient or inaccurate information for various reasons. Sometimes, the telephone consultation was too short to do justice to the problem; the clinician asked few or no questions to build rapport, obtain a full history, probe the patient’s answers for additional detail, confirm or exclude associated symptoms and inquire about comorbidities and medication. Video provided some visual cues but these were often limited to head and shoulders, and photographs were sometimes of poor quality.”
The additional burdens faced by patients and caregivers through use of virtual care was also identified. “Given the greater importance of the history in remote consultations, patients who lacked the ability to communicate and respond in line with clinicians’ expectations were at a significant disadvantage” the study states. “Several safety incidents were linked to patients’ limited fluency in the language and culture of the clinician or to specific vulnerabilities such as learning disability, cognitive impairment, hearing impairment or neurodiversity.
In a section on lessons to be learned from the study, the authors note that with virtual care relying more on history taking and dialogue, “verbal communication is even more mission critical.” They add that a final message from the analysis is that “clinical assessment provides less information when a physical examination (and even a basic visual overview) is not possible. Hence, the remote consultation has a higher degree of inherent uncertainty.”
In their summary of the article the authors give a shout out to front-line staff: “Rare safety incidents (involving death or serious harm) in remote encounters can be traced back to various clinical, communicative, technical and logistical causes. Telephone and video encounters in general practice are occurring in a high-risk (extremely busy and sometimes understaffed) context in which remote workflows may not be optimised. Front-line staff use creativity and judgement to help make care safer.”
(Graphic credit: HA.com)